The Evolution of Wireless Capsule Technology
Wireless capsule endoscopy (WCE) has emerged as a revolutionary approach to non-invasive medical diagnostics, offering a patient-centric alternative to traditional wired endoscopies. Since the first commercial capsule endoscope, the PillCam SB, gained FDA approval in 2001, this technology has witnessed remarkable advancements over the past two decades.
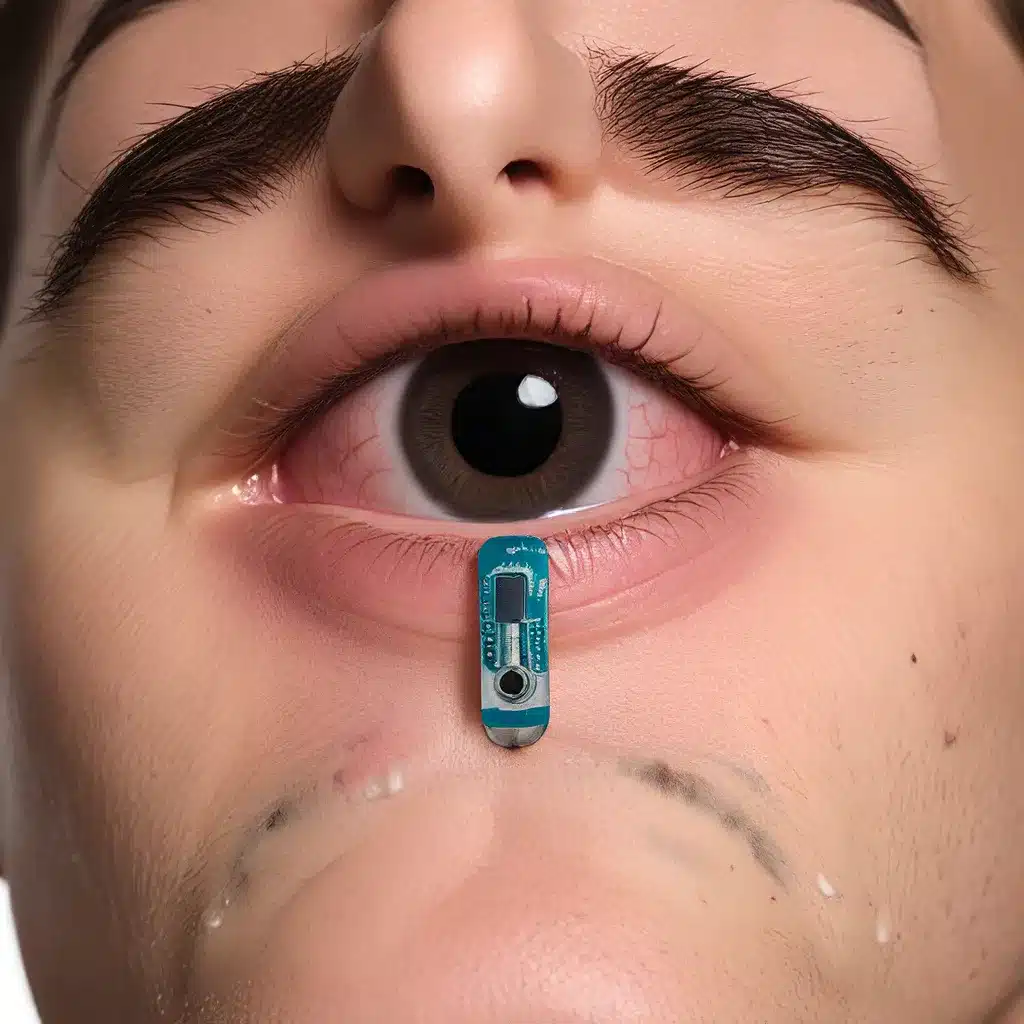
The core premise of WCE lies in its ability to capture high-resolution images of the gastrointestinal tract without the need for sedation or lengthy procedures. Patients simply swallow a small, pill-sized capsule that houses a camera, lighting, and wireless transmission components. As the capsule travels through the digestive system, it transmits real-time video data to an external receiver, enabling physicians to identify potential abnormalities for diagnosis.
Sensor networks and the Internet of Things (IoT) have played a pivotal role in driving the evolution of WCE. Innovations in micro-electromechanical systems (MEMS) fabrication, wireless communication, and artificial intelligence (AI) have unlocked new possibilities for enhancing the intelligence and functionality of these ingestible devices.
Expanding Capabilities: Towards the Capsule Surgeon
While the first-generation WCE devices revolutionized the field of gastrointestinal diagnostics, they were limited in their capabilities. These commercial capsules were primarily designed as passive video recorders, relying solely on the natural peristaltic motion of the digestive system for propulsion. They also lacked the ability to actively intervene or perform therapeutic procedures during examinations.
However, recent advancements in sensor technologies, wireless power transmission, magnetic control, and AI-driven image analysis have paved the way for a new generation of intelligent capsule robots. These “capsule surgeons” are envisioned to possess enhanced endurance, active locomotion, high-speed communication, precise positioning, autonomous lesion detection, and integrated diagnostic and therapeutic functionalities.
By incorporating these cutting-edge technologies, the capsule surgeon concept aims to supersede the limitations of traditional wired endoscopes and provide a comprehensive, minimally invasive solution for gastrointestinal examination and intervention.
Powering the Capsule Surgeon
One of the key challenges in the development of intelligent capsule robots is ensuring a reliable and efficient power supply. Existing commercial capsules typically rely on silver oxide button batteries, which can only sustain the device’s internal circuits for 8-10 hours. As the integration of additional functionalities, such as active locomotion and real-time data transmission, increases the power demand, the need for more advanced power sources becomes paramount.
Researchers have explored various alternatives to address this limitation, including:
- Custom-shaped lithium-ion polymer batteries: Offering higher power densities and longer runtime compared to traditional button cells.
- Self-powered batteries: Harnessing the energy from the digestive system’s gastric fluids to extend the capsule’s operational lifetime.
- Edible electronics: Leveraging innovative energy storage or harvesting techniques, such as edible batteries, supercapacitors, and nanogenerators, for improved safety and non-invasiveness.
However, these solutions still face challenges in terms of power output and integration within the limited space of the capsule.
Wireless Power Transmission: The Key to Untethered Mobility
To overcome the constraints of onboard power sources, wireless power transmission (WPT) has emerged as a promising solution for powering the capsule surgeon. This technology enables the transfer of electromagnetic energy from an external transmitter to a receiver embedded within the capsule, eliminating the need for a wired connection.
Two primary types of WPT are explored for WCE applications:
- Near-field transmission: Utilizes a small receiving coil within the capsule coupled with a larger transmitting coil on an external platform, enabling high-efficiency power transfer over short distances.
- Far-field transmission: Employs radiative electromagnetic waves to transmit power over longer ranges, but with lower efficiency.
Near-field WPT has garnered significant attention due to its ability to provide a reliable and efficient power supply to the capsule while minimizing its internal volume. This technology has demonstrated the potential to power the capsule’s internal components, including sensors, actuators, and communication modules, without compromising the device’s overall size and shape.
Active Locomotion: Enhancing Exploration and Control
Another crucial aspect of the capsule surgeon is its ability to actively navigate and maneuver within the gastrointestinal tract, in contrast to the passive, peristalsis-driven movement of commercial capsules.
Researchers have explored various approaches to achieve active locomotion, including:
- Shape memory alloy (SMA) actuators: Leveraging the shape-changing properties of SMAs to create legged or crawling mechanisms.
- Micro-motor propulsion: Utilizing miniature motors and propellers to generate thrust for forward movement.
- Magnetic field control: Employing external magnetic fields to wirelessly manipulate and steer the capsule’s motion.
Among these, magnetic field control has emerged as a particularly promising solution due to its contactless operation, durability, and reliability. By incorporating permanent magnets within the capsule and leveraging externally generated magnetic fields, physicians can remotely control the capsule’s position and direction, enabling a broader field of view and minimizing the risk of missed inspections.
Wireless Communication: Enabling High-Speed Data Transfer
Effective data transmission and reception are critical for the successful operation of the capsule surgeon. Conventional WCE devices typically rely on radio frequency (RF) communication, which faces challenges in providing the high data rates required for real-time video streaming and additional sensor data.
To address this limitation, researchers have explored alternative wireless communication technologies, including:
- Ultra-wideband (UWB): Offering superior transmission speeds exceeding 100 Mbps, UWB communication enhances video quality while reducing power consumption.
- Intrabody communication (IBC): Utilizing the human body as a conductive medium for data transmission, IBC provides a compact and energy-efficient alternative to RF-based systems.
These advanced wireless communication techniques enable the capsule surgeon to transmit high-resolution images, sensor data, and even control commands in a timely and reliable manner, facilitating remote diagnosis and intervention.
Precise Localization: Pinpointing the Capsule’s Position
Accurately determining the capsule’s position and orientation within the gastrointestinal tract is crucial for enabling targeted diagnostics and therapeutic procedures. However, the dynamic and complex nature of the digestive system poses significant challenges to achieving precise localization.
To address this, researchers have explored various positioning techniques, including:
- RF-based localization: Leveraging parameters such as received signal strength (RSS) and time of arrival (TOA) to estimate the capsule’s position.
- Magnetic localization: Employing an array of magnetoresistive sensors to detect the capsule’s magnetic field and determine its location and orientation.
- Video-based localization: Utilizing computer vision algorithms to analyze the capsule’s movement and position within the video frames.
By integrating these localization methods into a hybrid approach, the capsule surgeon can achieve highly accurate positioning, enabling physicians to pinpoint lesions and target specific areas for further investigation or treatment.
Intelligent Lesion Detection: Empowering Autonomous Diagnostics
One of the key capabilities of the capsule surgeon is its ability to autonomously detect and classify potential abnormalities or lesions within the gastrointestinal tract. This feature aims to alleviate the burden on medical professionals, who often face the time-consuming task of manually reviewing thousands of images captured during a WCE examination.
Advancements in AI-driven image analysis have been instrumental in addressing this challenge. Leveraging deep learning algorithms, the capsule surgeon can be trained to automatically identify and classify various types of lesions, including:
- Tumors: Detecting early-stage cancerous growths in the digestive system.
- Polyps: Identifying precancerous polyps for prompt intervention.
- Bleeding: Recognizing signs of gastrointestinal bleeding to enable timely diagnosis.
- Ulcers: Detecting inflammatory conditions like Crohn’s disease or ulcerative colitis.
By integrating these intelligent detection capabilities, the capsule surgeon can significantly reduce the time required for diagnosis, improve consistency in lesion identification, and enable more targeted and effective treatment strategies.
Integrated Diagnostic and Therapeutic Functions
Beyond its enhanced diagnostic capabilities, the capsule surgeon concept also aims to incorporate integrated therapeutic functionalities, eliminating the need for separate interventional procedures.
Researchers have explored various approaches to enable minimally invasive treatment within the capsule, including:
- Biopsy capabilities: Integrating micro-needles or scraping mechanisms to collect tissue samples for further analysis.
- Drug delivery: Leveraging magnetic fields or chemical reactions to trigger the release of targeted medications.
- Hemostatic interventions: Deploying clamps or other mechanisms to stop internal bleeding.
By seamlessly combining diagnostic and therapeutic features, the capsule surgeon can perform comprehensive examinations and execute necessary medical procedures without the need for additional surgical interventions, ultimately providing a more streamlined and patient-centric approach to gastrointestinal care.
Towards Clinical Integration: Addressing Challenges and Considerations
As the capsule surgeon concept gains momentum, it faces a myriad of challenges that must be addressed to ensure successful clinical integration and widespread adoption. These considerations span various aspects, including safety, regulatory compliance, data privacy, and ease of use.
Ensuring gastrointestinal safety: The integration of new technologies within the capsule must be carefully evaluated to mitigate risks of tissue damage, perforation, or obstruction. Strategies such as incorporating soft, deformable materials and leveraging magnetic fields for actuation can help address these concerns.
Meeting regulatory requirements: Obtaining regulatory approval for novel medical devices, like the capsule surgeon, requires extensive testing and compliance with established standards set by agencies such as the FDA and EMA. Comprehensive evaluation of factors like electromagnetic interference, specific absorption rate (SAR), and biocompatibility is essential.
Protecting patient data: With the increasing reliance on AI-driven image analysis and wireless data transmission, ensuring the security and privacy of patient medical information is paramount. Implementing robust data encryption protocols and exploring decentralized approaches, such as federated learning, can help address these challenges.
Enhancing user-friendliness: Integrating the capsule surgeon into clinical practice necessitates considering the ease of use for both medical professionals and patients. Developing intuitive control interfaces, such as teleoperation or virtual reality-based systems, can streamline the integration of these sophisticated devices into the healthcare ecosystem.
By proactively addressing these multifaceted challenges, the research community and medical practitioners can pave the way for the successful clinical translation of the capsule surgeon, unlocking new frontiers in minimally invasive gastrointestinal diagnostics and therapeutics.
Conclusion: The Future of Sensor-Driven Medical Robotics
The evolution of wireless capsule endoscopy has been a remarkable testament to the transformative power of sensor technologies and the Internet of Things. From passive video recorders to the envisioned capsule surgeon, this field has witnessed a remarkable progression, driven by advancements in areas such as wireless power transmission, active locomotion, high-speed communication, precise localization, and AI-powered image analysis.
As the capsule surgeon concept continues to mature, it holds the promise of revolutionizing the way we approach gastrointestinal diagnostics and interventions. By seamlessly integrating diagnostic and therapeutic functionalities within a compact, swallowable device, these intelligent capsule robots have the potential to deliver a more comprehensive, patient-centric, and minimally invasive approach to healthcare.
Looking ahead, the convergence of sensor networks, robotics, and biomedical engineering will undoubtedly shape the future of medical technology, paving the way for innovative solutions that redefine the boundaries of what is possible in the realm of sensor-driven medical diagnostics and therapeutics.